Zygomatic Implants and the ZAGA Concept
Welcome to our informative guide on zygomatic implants. This innovative treatment is specifically designed for patients who have been told they have insufficient bone for traditional dental implants. If you’re exploring options for dental implants but face challenges due to bone loss in the jaw, zygomatic implants may be a suitable solution for you. This guide will help you understand how these implants can provide a reliable alternative for enhancing your smile.
We use scientific research data and information from various studies, which you can find at zagacenters.com. This helps us explain how the ZAGA Technique can benefit dental patients. The technique provides a reliable long-term solution for patients who have been told they are not suitable candidates for traditional dental implants or those seeking improved dental care.
Home » Frequently Asked Questions » What are the ZAGA Concept and Zygomatic Implants ?
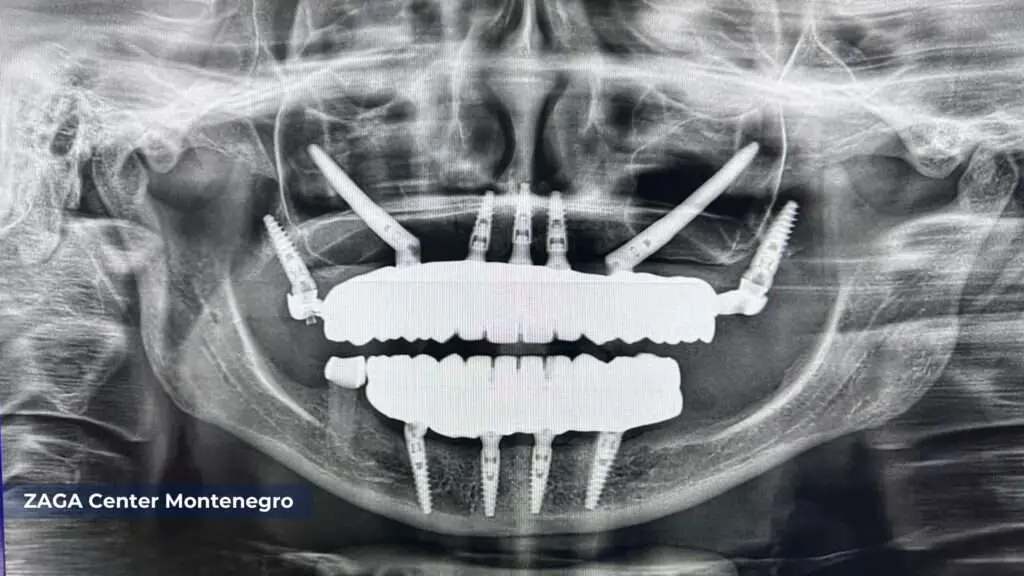
Table of Contents
Understanding Severe Maxillary Atrophy
Severe maxillary atrophy is a critical condition characterized by the extensive loss of bone in the upper jaw. It can occur due to prolonged tooth loss, trauma, infections, or medical conditions like osteoporosis. This significant bone deterioration not only affects a person’s ability to chew, speak, and maintain facial aesthetics but also makes it extremely challenging to support dental prosthetics with traditional implants. In many cases, patients with severe maxillary atrophy are told they are not suitable candidates for conventional implant procedures due to the lack of sufficient bone structure. Understanding the complexities of this condition is essential for both patients and professionals, as it opens the door to innovative solutions such as zygomatic implants. These advanced treatments offer renewed hope for full oral rehabilitation, bypassing the need for bone grafts and providing a stable foundation for dental restorations.
Introducing Zygomatic Implants
Zygomatic implants have revolutionized the field of dentistry by offering a breakthrough solution for patients with severe maxillary atrophy, who will be perfect candidates for zygomatic implants. Surgeons insert zygomatic implants in the cheekbone for support, and place regular implants in the jawbone. This technique provides a stable foundation for dental prosthetics, ensuring optimal functionality and aesthetics.
Zygomatic implants are for people with insufficient upper jaw bone for regular dental implants. Imagine your jawbone as the soil in a garden.
Just like certain plants need deep soil to grow well, regular dental implants need a good amount of bone to hold onto. But what if the soil (or bone) isn’t deep enough? That’s where zygomatic implants come in.
Zygomatic implants are longer and anchor into the cheekbone instead of the jawbone for better stability. The cheekbone is usually much stronger and has more depth than the upper jawbone, making it a great foundation for these implants.
Here’s a simple breakdown:
- Traditional Dental Implants: Need a good amount of jawbone to attach to.
- Zygomatic Implants: Don’t rely on jawbone depth. They anchor into the cheekbone, offering a solution for those with less jawbone.
Zygomatic implants help people with not enough bone for regular implants get fixed teeth. They can now enjoy the benefits of having permanent teeth. It’s like planting a tree in shallow soil with a strong support that reaches a solid foundation for stability and growth.


The Benefits of Zygomatic Implants
- Immediate Results: One of the key advantages of zygomatic implants is their ability to provide immediate functionality. Zygomatic implants can fix your smile in just one dental implant procedure. Patients must wait several months for traditional implants to heal before the dentist can add the final prosthetics. While zygomatic implants support immediate loading, they still require a period for osseointegration, where the implant integrates with the bone. This process is crucial for long-term stability and typically takes several months, similar to traditional implants. However, the initial stability provided by the zygomatic bone allows patients to have functional teeth during this integration period. (1)
- Avoidance of Bone Grafting: Severe maxillary atrophy often requires extensive bone grafting procedures to augment the jawbone. However, zygomatic implants can eliminate the need for such interventions as they are attached to the cheekbone (2). This reduces treatment time and avoids additional surgical procedures, making the process more convenient and less invasive.
- Severe maxillary atrophy can make it hard to chew and enjoy different foods. Restoring the chewing function can help with this, as zygomatic implants give strong support, helping patients eat normally again.
- Severe maxillary atrophy may cause a sunken facial appearance, which can diminish confidence in one’s appearance. Zygomatic implants can make your face look better and give you more confidence by fixing your smile and providing structural support to your face. (4)
The ZAGA Technique: A Pioneering Approach
The ZAGA Technique is a pioneering approach in zygomatic implantology. The “Zygoma Anatomy-Guided Approach” is the treatment known for fitting each patient’s unique anatomy through personalization. This approach uses advanced dental implant technology to achieve the best results, involving meticulous surgery planning and precise implant placement based on the individual’s zygomatic bone structure (5).
By utilizing the ZAGA Concept, dental professionals can achieve the following benefits:
- The ZAGA Technique focuses on patient-centered care. It prioritizes the patient’s needs and takes into account their individual anatomy. This approach enables the development of a personalized treatment plan, which increases the chances of highly successful outcomes.
- The ZAGA Technique plans and places zygomatic implants carefully. This ensures minimally invasive treatment with predictable results and lasting outcomes. Patients can have peace of mind about their treatment.
- Simpler Surgery: The ZAGA Technique focuses on each patient’s anatomy, making surgery less complex. This leads to quicker and more efficient surgeries.
- The ZAGA Technique reduces complications during zygomatic implant surgery. It considers bone and anatomical factors to lower the risk of problems. This technique helps to minimize potential issues that may arise during the surgery. By taking these factors into account, the ZAGA Technique improves the overall success rates and safety of the procedure. (6)


Conclusion
For dental patients suffering from severe maxillary atrophy, zygomatic implants offer a revolutionary solution that can restore oral health, functionality, and self-confidence. With their immediate functionality, avoidance of bone grafting, restored chewing function, and enhanced aesthetics, zygomatic implants can significantly improve the quality of life of edentulous patients.
The ZAGA Technique, with its patient-centric approach and predictable outcomes, further enhances the success of zygomatic implant treatments.
Consult our Smile 24h doctors and dental professionals trained in the ZAGA Technique to improve your smile. This technique can help you begin a journey towards a better smile.
References:
Aparicio, C., Dawood, A., Ucer, C. (2023). Zygomatic Implants. The ZAGA Concept. In: Rinaldi, M. (eds) Implants and Oral Rehabilitation of the Atrophic Maxilla. Springer, Cham.
Solà Pérez A, Pastorino D, Aparicio C, Pegueroles Neyra M, Khan RS, Wright S, Ucer C. Success Rates of Zygomatic Implants for the Rehabilitation of Severely Atrophic Maxilla: A Systematic Review. Dent J (Basel). 2022 Aug 12;10(8):151.
Aparicio, C., Polido, W.D., Chow, J. et al. Round and flat zygomatic implants: effectiveness after a 1-year follow-up non-interventional study. Int J Implant Dent 8, 13 (2022).
Aparicio, C., Olivo, A., de Paz, V. et al. The zygoma anatomy-guided approach (ZAGA) for rehabilitation of the atrophic maxilla. Clin Dent Rev 6, 2 (2022).
Aparicio C, López-Píriz R, Peñarrocha M. Preoperative Evaluation and Treatment Planning. Zygomatic Implant Critical Zone (ZICZ) Location. Atlas Oral Maxillofac Surg Clin North Am. 2021 Sep;29(2):185-202.
Aparicio C, Polido WD, Zarrinkelk HM. The Zygoma Anatomy-Guided Approach for Placement of Zygomatic Implants. Atlas Oral Maxillofac Surg Clin North Am. 2021 Sep;29(2):203-231.
Aparicio C, Polido WD, Chow J, David L, Davo R, De Moraes EJ, Fibishenko A, Ando M, Mclellan G, Nicolopoulos C, Pikos MA, Zarrinkelk H, Balshi TJ, Peñarrocha M. Identification of the Pathway and Appropriate Use of Four Zygomatic Implants in the Atrophic Maxilla: A Cross-Sectional Study. Int J Oral Maxillofac Implants. 2021 Jul-Aug;36(4):807-817.
Clarós, P. & Końska, N. & Clarós-Pujol, P. & Sentís, J. & Clarós, Pedro & Penarrocha, Miguel & Aparicio, Carlos. (2021). Prevalence of maxillary sinus alterations after zygomatic surgery. A comparative study between intra-sinus and ZAGA approaches. Dentistry and Oral Maxillofacial Surgery.
Aparicio C, López-Piriz R, Albrektsson T. ORIS Criteria of Success for the Zygoma-Related Rehabilitation: The (Revisited) Zygoma Success Code. Int J Oral Maxillofac Implants. 2020 Mar/Apr;35(2):366-378.
Aparicio C, Antonio S. Zygoma Anatomy-Guided Approach “Scarf Graft” for Prevention of Soft Tissue Dehiscence Around Zygomatic Implants: Technical Note. Int J Oral Maxillofac Implants. 2020 Mar/Apr;35(2):e21-e26
M PD, Jc BM, A FR, C A, D PO. Bone Regeneration and Soft Tissue Enhancement Around Zygomatic Implants: Retrospective Case Series. Materials (Basel). 2020 Mar 29;13(7):1577
Aparicio C, Manresa C, Francisco K, Claros P, Alández J, González-Martín O, Albrektsson T. Zygomatic implants: indications, techniques and outcomes, and the zygomatic success code. Periodontol 2000. 2014 Oct;66(1):41-58.
Aparicio C, Manresa C, Francisco K, Aparicio A, Nunes J, Claros P, Potau JM. Zygomatic implants placed using the zygomatic anatomy-guided approach versus the classical technique: a proposed system to report rhinosinusitis diagnosis. Clin Implant Dent Relat Res. 2014 Oct;16(5):627-42.
Aparicio C, Manresa C, Francisco K, Ouazzani W, Claros P, Potau JM, Aparicio A. The long-term use of zygomatic implants: a 10-year clinical and radiographic report. Clin Implant Dent Relat Res. 2014 Jun;16(3):447-59.
Aparicio, Carlos. (2011). A proposed classification for zygomatic implant patient based on the zygoma anatomy guided approach (ZAGA): a cross-sectional survey. European journal of oral implantology. 4. 269-75.
Aparicio C, Ouazzani W, Aparicio A, Fortes V, Muela R, Pascual A, Codesal M, Barluenga N, Franch M. Immediate/Early loading of zygomatic implants: clinical experiences after 2 to 5 years of follow-up. Clin Implant Dent Relat Res. 2010 May;12 Suppl 1:e77-82.
Aparicio C, Ouazzani W, Aparicio A, Fortes V, Muela R, Pascual A, Codesal M, Barluenga N, Manresa C, Franch M. Extrasinus zygomatic implants: three year experience from a new surgical approach for patients with pronounced buccal concavities in the edentulous maxilla. Clin Implant Dent Relat Res. 2010 Mar;12(1):55-61.
Aparicio C, Ouazzani W, Hatano N. The use of zygomatic implants for prosthetic rehabilitation of the severely resorbed maxilla. Periodontol 2000. 2008;47:162-71.
Aparicio C, Rangert B, Sennerby L. Immediate/early loading of dental implants: a report from the Sociedad Española de Implantes World Congress consensus meeting in Barcelona, Spain, 2002. Clin Implant Dent Relat Res. 2003;5(1):57-60.
Aparicio C, Ouazzani W, Garcia R, Arevalo X, Muela R, Fortes V. A prospective clinical study on titanium implants in the zygomatic arch for prosthetic rehabilitation of the atrophic edentulous maxilla with a follow-up of 6 months to 5 years. Clin Implant Dent Relat Res. 2006;8(3):114-22.
Carlos Aparicio, MD, DDS, DLT, MS/Per-lngvar Brånemark, MD, PhD/Eugene E. Keller, DDS, MSD/Jordi Olivé, MD, DDS, DUPMF. Reconstruction of the Premaxilla With Autogenous lliac Bone in Combination With Osseointegrated Implants. International Journal of Oral & Maxillofacial Implants. Volume 8 , Issue 1. January/February 1993. Pages 61-67






